FlexPasser™
For Retrieval of Retracted Proximal Tendons
The FlexPasser Tendon Retrieval Kit provides a system of single use instrumentation for the retrieval of the retracted proximal tendon stump(s) during the repair of lacerated digital flexor tendon(s) in the hand.
-

Retrieve retracted tendon end with minimal incisions
-

Reduce the risk of damage to tendon end compared to standard technique*
-

Avoid the need for repeat suturing of the tendon end
Surgery to repair lacerated or severed flexor tendons in the hand can lead to additional trauma to the tendon end or tendon sheath which may cause adhesion post-operatively. This trauma and possible adhesion can reduce the range of movement and impair the outcome of the surgery (1,2,3).
INDICATIONS
The FlexPasser Tendon Retrieval Kit is intended for use in the retrieval of the proximal tendon stump(s) during the repair of a lacerated digital flexor tendon(s) in the hand.
HOW DOES IT WORK?
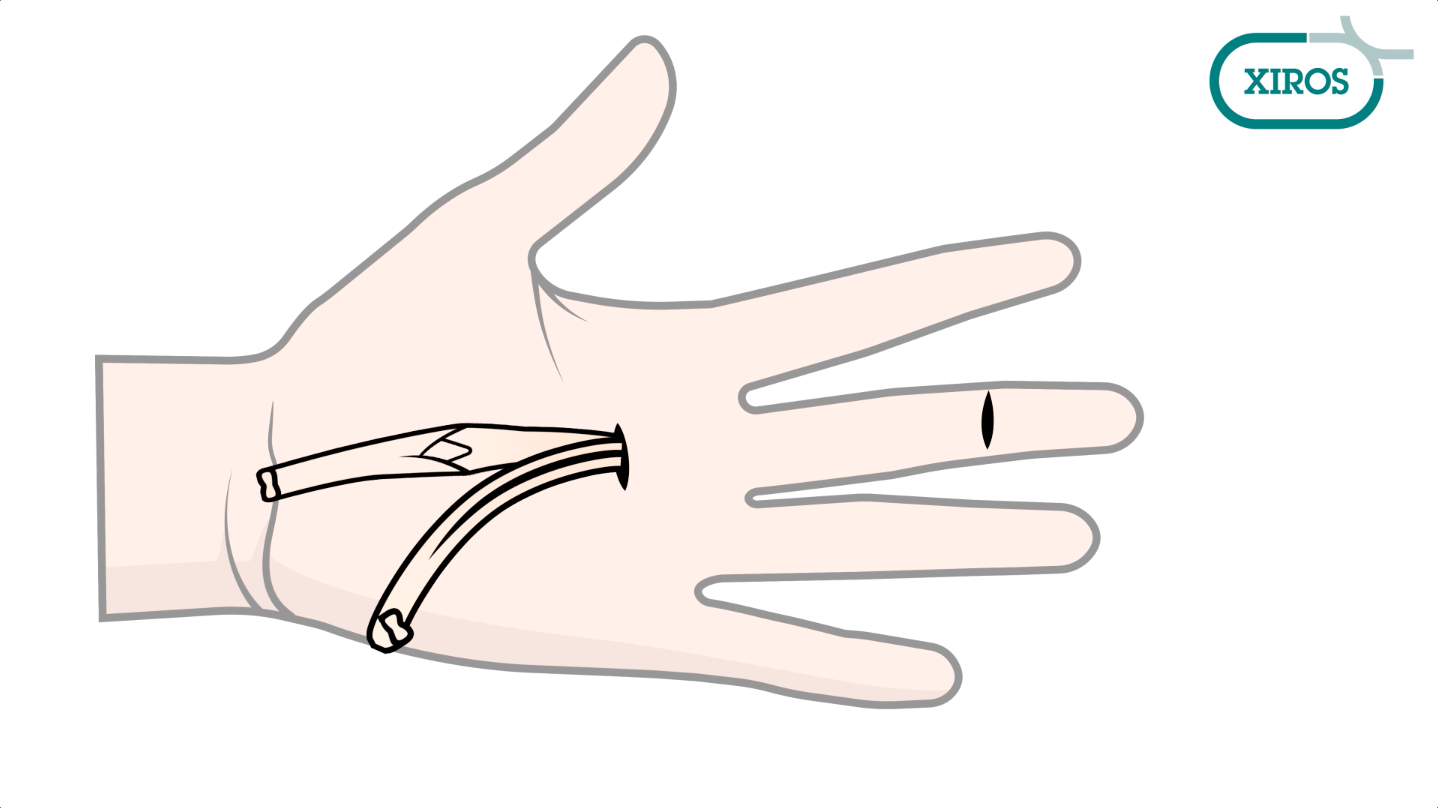
- The proximal tendon stump is delivered to the palm via a small incision in the crease of the palm (Figure A), or proximal point of choice if the vinculum is to be preserved. The palm is preferred, to minimise incisions on the digit.
- The finger should be gently extended. The probe is advanced with its round end leading through the flexor sheath, from the site of the distal flexor stump/opening in the sheath to the site of the proximal flexor stump. Hold the device close to the tip and advance in stages, maintaining the orientation of the probe to avoid buckling and rotation (Figure A).
- Maintain the probe’s orientation as it is pulled through the proximal incision (Figure B), leaving the plastic sleeve in place protruding from both incisions, ensure the sleeve has not twisted before proceeding.
- The full thickness of one leg of the sleeve is cut across obliquely (Figure B) at the base of the tapered segment. The oblique cut creates a larger entry point for the tendon than a transverse cut.
- The leg that has not been cut can be removed from the digit, leaving a single sleeve in place (Figure C).
- The proximally retracted flexor tendon stump is sutured using the surgeon’s preferred technique for the repair, leaving the suture ends long enough for retrieval. The needle is to be kept on the suture (Figure D).
- The free end of the suture is introduced into the open end of the needle carrier to about 4-5 cm. Then, using a needle holder, the entire body of the curved needle is introduced in the carrier antegrade (Figure D), gently curving the carrier to preserve the needle tip.
- The Integrated probe and needle carrier is threaded through the plastic sleeve from the proximal to distal incisions and removed at the distal incision (Figure E), once the needle and suture have been passed through the sleeve they can be released from the carrier (Figure F).
- We recommend that a small volume of saline should be used to lubricate the sleeve and tendon prior to passing the tendon through the plastic sleeve lining the sheath. Gentle traction is applied to both ends of the suture (Figure F), whilst the plastic sleeve is held in place with forceps at the proximal incision, to guide the proximal tendon stump(s) through the cavity of the sleeve and to the distal wound (Figure F).
- Keeping tension on the suture, the sleeve is then pulled from the distal wound out of the tendon sheath thus freeing both ends of the suture in readiness for the tendon repair.
- The two stumps can now be connected by continuing the chosen repair technique with the same needle and suture material.
- If the FDP and FDS both require repair, then they should be placed in the anatomic orientation prior to proceeding as per steps 6 – 10. One suture pair at a time should be passed through the plastic sleeve. Then the four suture strands are used to draw the two tendons simultaneously to the distal incision where each can be sutured to its own stump.
ORDER NUMBERS
- 202-1500 – FlexPasser™ Tendon Retrieval Kit
Features and Benefits
- For atraumatic retrieval of severed flexor tendons with minimal incisions.
- Retrieve retracted tendon end with minimal incisions.
- Reduce the risk of damage to tendon end compared to standard technique*
- Avoid the need for repeat suturing of the tendon end.
* Based on cadaver trials
Additional Information
Please note: Regulatory approval for products mentioned on this website varies from country to country. For further information, and for details of local distributors and agents, contact our Sales and Marketing team at enquiries@xirosna.com. All data listed on this page is held at Xiros and can be requested by contacting enquiries@xirosna.com.
 Xiros
Xiros